Osteoporosis: Strengthen bones. Prevent falls.
Osteoporosis is surprisingly common and frequently results in broken bones. But there are things you can support your loved one to do to strengthen bones. Also to protect against falls, the most common cause of a bone fracture.
Signs of osteoporosis
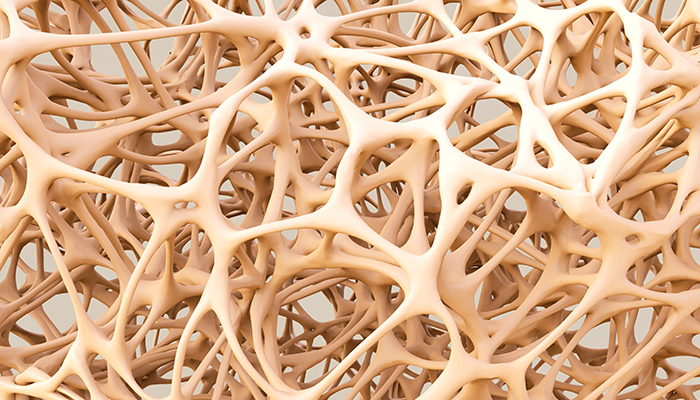 Does the person you care for seem to have shrunk a bit? Pants are too long? Can’t reach items on their regular shelf? They may have osteoporosis, a condition where bones become more porous with age.
Does the person you care for seem to have shrunk a bit? Pants are too long? Can’t reach items on their regular shelf? They may have osteoporosis, a condition where bones become more porous with age.
With osteoporosis, bones are less dense and easily develop cracks and fractures that may or may not be painful. When cracks occur in the spinal column, the spine compresses, resulting in shortened height. In some people, the compression produces a hump or curve at the neck and shoulders. In other parts of the body, such as the hips, poor bone density is not obvious until a bone is broken.
Osteoporosis is serious, but underdiagnosed. Every year, about 2 million people over age 50 break a bone because of osteoporosis. For those who break a hip
- 50% will need to use a walker or cane, at least temporarily
- 25% will require some form of care assistance long term
- 25% will not recover (the broken bone leads to a cascade of problems that ultimately results in death within a year).
Those most at risk are
- women older than age 50. One out of two is likely to break a bone because of osteoporosis. (One in four men over 50 will break a bone. More for those over 70.)
- people of slight build
- people of Caucasian and/or Asian descent
- those with a family history of osteoporosis
There are lifestyle risks as well, including smoking, drinking alcohol, and not exercising.
Getting tested
If your loved one complains about back pain, seems shorter, or has any of the known risk factors, ask the doctor about doing a bone density test. This specialized x-ray test (often called a “DEXA scan”) measures the thickness of the hip and sometimes other bones. Some cases might require an MRI. Medicare will usually pay for these tests if a doctor orders them.
Osteoporosis: What you can do

If you are concerned about a loved one’s osteoporosis—brittle bones—it’s a good idea to bring this up with the doctor. He or she will likely discuss various medicines that can help. In addition, changes in daily life outlined below can go a long way to making stronger bones. Consider:
Diet: There are two key nutrients.
- The best food sources are low-fat dairy products; dark green leafy vegetables; canned salmon, mackerel, or sardines (with bones); and tofu. Women over age 50 should consume a total of 1200 mg of calcium per day. Men need 1000 mg/day until age 70. Then they too should get 1200 mg/day. A supplement is fine. But be sure to pick a dose that factors in the calcium your relative already receives from food. More than 2000 mg/day may increase the risk of heart disease and kidney stones.
- Vitamin D. Exposure to sunshine yields vitamin D. But only when sunscreen is not used (no free lunch!). Look for foods such as milk that have been fortified with vitamin D. Or get a supplement. Adults age 51–70 are advised to take 600 international units (iu)/day. Those age 71 and over need 800 iu/day. African Americans don’t absorb vitamin D well through the skin, so 2000 iu is the recommended supplement. Most people can safely take up to 4000 iu/day.
Strength exercises. Weight-bearing exercise works with gravity to produce strong bones: Brisk walks, hiking, dancing, climbing up stairs. Resistance training also helps: Lifting weights or using exercise bands. Talk to the doctor about the safest way to build up strength.
Lifestyle changes
- Get up off the couch! A sedentary lifestyle leads to brittle bones.
- Limit alcohol to no more than two drinks/day. Alcohol kills bone cells and leaches calcium from the bones.
- Stop smoking. Smokers’ bones heal more slowly.
Addressing the risk of a fall
The biggest danger of osteoporosis is a broken bone due to a fall. Each year one out of four adults 65 and over falls, making falls the leading cause of injury for older adults.
Falls are serious business. In the United States an older adult dies once every 20 minutes as a result of a fall. Disabilities from a fall include injuries that can be life changing: A traumatic brain injury or broken hip. Especially for seniors, falls pose a danger to independence, bringing on a permanent need for daily help.
Who is at risk for falling? Has Mom or Dad fallen twice in the past year? Have you noticed balance or gait problems? Has there recently been a severe fall? These are signs of “high risk.” Other signs involve poor vision or taking medicines that list dizziness as a side effect.
A fall-risk assessment. To be safe, ask your relative’s doctor to do a fall-risk assessment. This includes a review of
- underlying medical conditions. Many chronic diseases affect the ability to get around;
- the home environment. The doctor can write an order for an occupational therapist or other trained professional to do a home assessment. They can identify simple ways to remove hazards;
- medication use. Some drugs, or daily use of four or more prescription drugs, increase the risk for falling.
Preventing falls. A recent review of numerous studies shows that some strategies are better than others. The most effective include
- exercise, especially activities that promote balance
- getting regular eye exams and following through with corrective procedures
- removing hazards around the house
- wearing sturdy shoes and slippers. A firm sole is better than a soft cushy one because it’s easier to feel the ground below
Contact us at (707) 364-5285
